Pioneering Cancer Immunotherapy: Harnessing the Power of the Immune System
Dr PP Devan +91 92433 01213
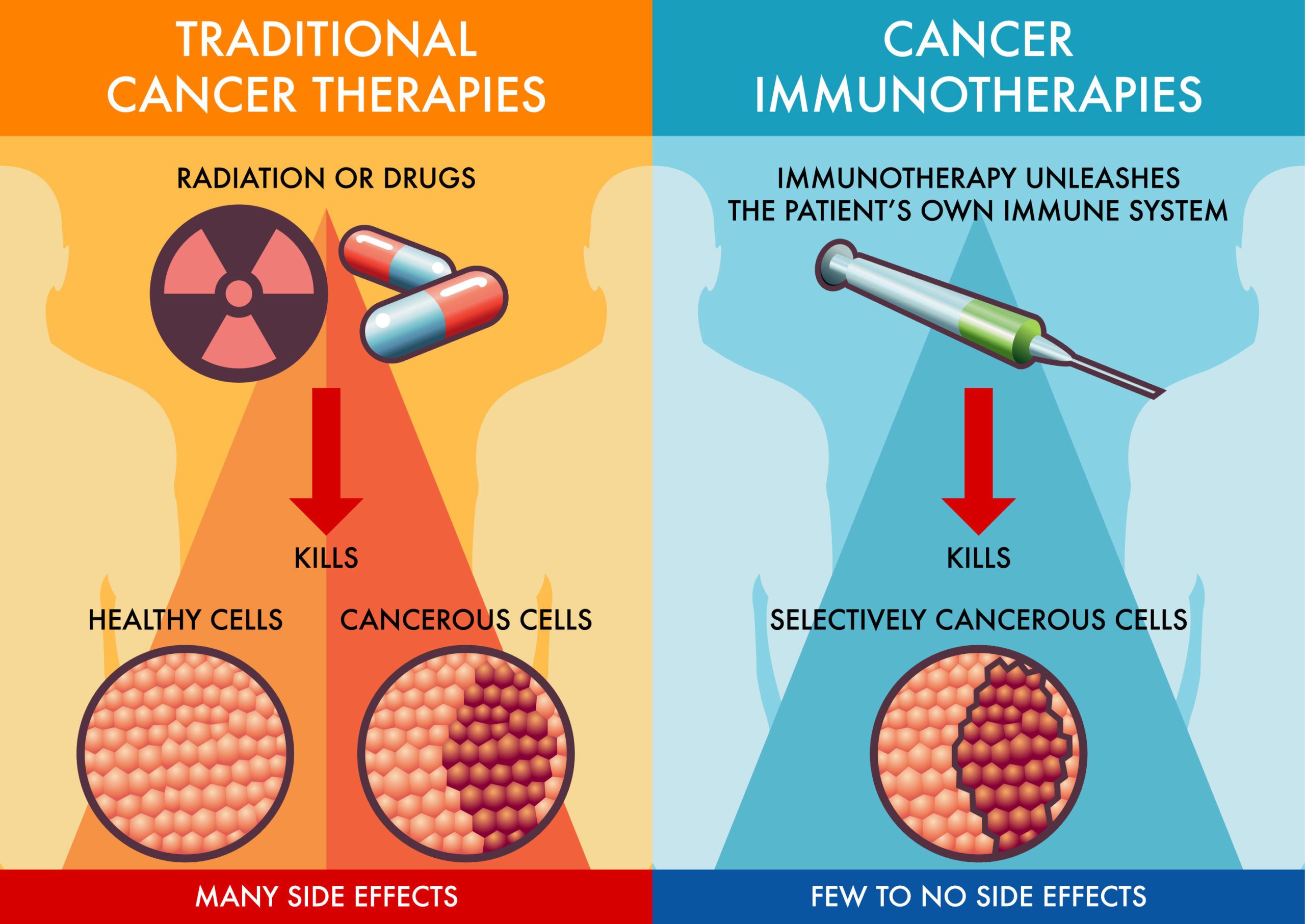
Cancer remains one of the most formidable challenges in modern medicine, with conventional treatments often posing significant side effects and limited efficacy. However, the advent of cancer immunotherapy has revolutionized treatment paradigms by leveraging the body’s own immune system to combat cancer cells effectively. The principles, advancements, and promising outcomes of cancer immunotherapy, highlightS its transformative impact on cancer treatment.
Understanding Cancer Immunotherapy
Cancer immunotherapy operates on the principle that the immune system can be stimulated or augmented to recognize and destroy cancer cells more effectively. Unlike traditional treatments such as chemotherapy and radiation, which directly target cancer cells, immunotherapy enhances the body’s natural defenses to fight cancer.
Types of Cancer Immunotherapy
Checkpoint Inhibitors: These drugs block inhibitory pathways (like PD-1/PD-L1 or CTLA-4) that cancer cells use to evade detection by the immune system. By “releasing the brakes” on immune cells, checkpoint inhibitors restore their ability to recognize and attack cancer cells.
CAR T-cell Therapy: Chimeric Antigen Receptor (CAR) T-cell therapy involves modifying a patient’s T-cells to express receptors that can identify specific proteins on cancer cells. These engineered T-cells are then reintroduced into the patient’s body to target and destroy cancer cells.
Cancer Vaccines: Cancer vaccines work by stimulating the immune system to recognize and attack cancer cells. These vaccines can be made from cancer cells, parts of cells, or specific proteins found on cancer cells. They are designed to train the immune system to recognize cancer cells as foreign invaders.
Monoclonal Antibodies: Monoclonal antibodies are laboratory-produced molecules that can bind to specific targets on cancer cells. They can be used to directly kill cancer cells, block growth signals, or deliver drugs or radiation directly to cancer cells.
Personalized Medicine and Success Stories
One of the most remarkable aspects of cancer immunotherapy is its potential for personalized medicine. By tailoring treatments to a patient’s immune profile and specific cancer characteristics, immunotherapy offers a targeted and potentially more effective approach than traditional treatments.
Numerous success stories underscore the transformative impact of cancer immunotherapy. Patients with advanced melanoma, lung cancer, and leukemia, among others, have experienced durable responses and even complete remissions after failing to respond to conventional therapies. These outcomes highlight the power of harnessing the immune system’s inherent ability to recognize and eliminate cancer cells.
Challenges and Future Directions
Despite its promise, cancer immunotherapy faces challenges such as identifying biomarkers to predict treatment response, managing immune-related side effects, and overcoming resistance mechanisms developed by cancer cells. Ongoing research aims to address these challenges and expand the application of immunotherapy to a broader range of cancers and patient populations.
cancer immunotherapy represents a paradigm shift in the treatment of cancer, offering new hope and improved outcomes for patients worldwide. By empowering the immune system to combat cancer cells more effectively, immunotherapy not only enhances treatment efficacy but also reduces the systemic toxicity associated with traditional therapies. As research continues to advance and new innovations emerge, the future of cancer treatment looks increasingly promising with immunotherapy at its forefront. Embracing these advancements in oncology underscores a commitment to personalized, targeted therapies that hold the potential to transform the landscape of cancer care in the years to come.





